Abstract
Introduction :
Adult' autoimmune hemolytic anemia (AIHA) can be life-threatening with an overall mortality rate of 8-10% which can rise up to 30% for patients admitted in intensive care unit (ICU). The factors associated with the need of management in ICU are partially unknown as only few data are available in the literature. To better describe the baseline characteristics and outcome of severe adult'AIHA admitted in ICU and to identify some prognostic factors, an observational multicentre study was set up by the French reference center of adult' immune cytopenias.
Patients and Methods :
This was an observational retrospective multicentre study. Patients had to fulfill the following inclusion criteria : 1) Age ≥ 18 years at time of AIHA onset ; 2) Definite diagnosis of primary or secondary warm (wAIHA), cold (cAIHA) or mixed AIHA ; 3) At least one admission in ICU specifically for the management of AIHA. Patients with AIHA admitted in ICU for another reason than the severity of AIHA were excluded. Patients' baseline characteristics at time of admission in ICU were recorded by means of a standardized form including the Charlson comorbidity score, the Knaus score, the Sequential Organ Failure Assessment (SOFA) and the Simplified Acute Physiology Score (SAPS II). Categorical variables were expressed as number (percentage) and quantitative variable as median [interquartile range]. To identify factors associated with death in ICU or after 1 year of follow-up, patients' characteristics were compared using usual tests. In order to identify some parameters associated with the risk of admission in ICU, the main characteristics of the patients were compared to those of controls (1 to 2 ratio) diagnosed with AIHA and followed over the same period who were never admitted in ICU. Univariate logistic regressions analyses were performed followed by a multivariate logistic regression using a backward stepwise selection procedure. A p-value <0.05 was considered as statistically significant.
Results :
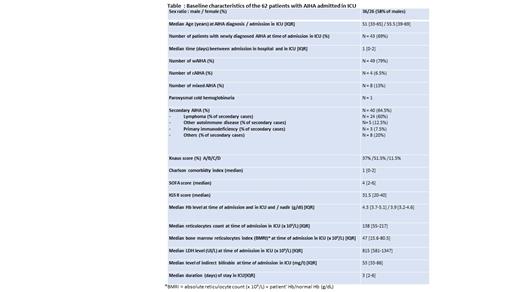
In total, 62 patients (42% of females) from 11 centers fulfilling the inclusion criteria were included for a total of 69 admissions in ICU (see table for baseline characteristics). Of note, 57/62 patients (92%) had a low (< 121) bone marrow reticulocytes index (BMRI) reflecting an impaired erythropoiesis. The mortality rate in ICU was 13%; 3 patients died from massive pulmonary embolism. Compared to the 54 survivors the 8 patients who died in ICU had: a higher CRP level (p value = 0.011); a higher need for transfusion (median number of packed red cells was 12 versus 4, p value = 0.008); higher SOFA and IGS scores (p value = 0.006); a higher number of organ failures on admission (p value < 0.001), thrombotic events (p value = 0.024) and sepsis during the stay in ICU (p value = 0.019). Among the survivors, 9/49 (5 lost of follow-up) eventually died within a year after the admission in ICU leading to an overall mortality rate of 30% at 1 year. For the management of AIHA in ICU, 56 patients (90%) were transfused (median number of packed red cells = 4 [2-7]); recombinant Epo was administered to 14 patients (22.5%) and 5 patients (8%) had plasma exchange. In ICU, 58 patients (95%) were treated with corticosteroids, 29 (46%) received at least one other treatment line including mostly : rituximab (n = 22), intravenous immunoglobulin (n = 10), iv cyclophosphamide (n = 5), cyclosporin (n = 3). Other treatment lines including chemotherapy-based regimen (n=8) were given afterwards. The characteristics of the 62 patients were compared to those of 138 controls with AIHA who were never admitted in ICU. In univariate analyses, younger age, Evans' syndrome, Hb level < 6 g/dl; reticulocytes count < 100 x 10 9/L, BMRI <121 and high bilirubin level were significantly associated with an admission in ICU. In multivariate analysis, a low Hb level and a high bilirubin level were the only parameters that were significantly associated with the risk of admission in ICU
Conclusion :
Based on this retrospective study, the mortality rate of adult patients admitted in ICU for AIHA was lower than expected (13%) but the 1 year mortality rate in this population of patients rose up to 30%. Patients with AIHA and a Hb level < 6g/dl, a high bilirubin level and/or an inadequate reticulocytes count must be treated promptly and monitored closely beyond the initial phase of the disease in order to reduce the mortality rate. The treatment of severe refractory cases is not consensual and should be harmonized.
Comont: Takeda: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Bristol Myers Squibb: Honoraria, Research Funding; AstraZeneca: Honoraria, Research Funding; Abbvie: Honoraria, Research Funding. Riviere: Octapharma: Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees. Haioun: Janssen: Honoraria, Research Funding; Gilead: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; F. Hoffmann-La Roche Ltd: Honoraria, Research Funding; Servier: Honoraria, Research Funding; Takeda: Honoraria, Research Funding; Miltenyi: Honoraria, Research Funding. Godeau: Amgen: Consultancy; Sobi: Consultancy; Novartis: Consultancy; Grifols: Consultancy. Michel: Amgen: Consultancy; Rigel: Honoraria; Alexion: Honoraria; UCB: Honoraria; Argenx: Honoraria; Novartis: Consultancy.
rituximab is commonly used off-label as a second line for adult' AIHA

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal